The right kind of doctors for Texas

Revisiting barriers to building the primary care workforce, 20 years later
By Kate Alfano
For 20 years, health care stakeholders have urged academic institutions to change how they educate medical students and how they distribute funding within their graduate medical education programs in order to advance the training of more primary care physicians. Despite compelling and conclusive evidence that shows patients with ready access to primary care receive higher quality care with better health outcomes for less cost, the players best able to turn the downward trend in the primary care physician workforce have failed to enact meaningful reforms.
In the early 1990s, when the current class of first-year medical students were babies and toddlers, the Texas Academy of Family Physicians released two reports—“Training Family Physicians: A Vital Element in Solving Texas’ Access to Health Care Crisis”(1) and “The Right Kind of Doctors for Texas: A Strategy for Meeting Physician Workforce Needs of Texas”(2)—that warned of an impending primary care physician shortage and outlined recommendations to correct the disparities in specialty mix and geographic distribution.
Similarly, the Council on Graduate Medical Education published its Third Report(3) in October 1992 that described the crisis in health care delivery on the national level. The authors called on educational institutions to be more responsive to the public need for more practicing primary care physicians, underrepresented minority physicians, and physicians more likely to practice in underserved rural and inner-city areas. They called for the development of a national workforce plan and strategy in medical education financing and health care payment systems that would remove barriers to training and improve access to primary care.
COGME revisited these issues in its Twentieth Report,(4) published in December 2010, more directly calling on institutions to produce more primary care physicians, deconstruct the barriers to a primary care-based workforce, and address a number of issues: decreased interest in primary care professions, the mechanisms of physician payment and need for practice transformation in primary care, the biased premedical and medical school environment, issues in the graduate medical education environment, and the geographic and socioeconomic maldistribution of physicians.
Yet, even with reams of studies from respected organizations and policy experts calling for a health care system grounded in primary care, academic institutions today still lag far behind in producing enough primary care physicians to care for a population that is rapidly growing, aging, and presenting worse and more complex health conditions.
Considering that graduate medical education is not a single entity, but rather the sum of the accreditation and certification organizations, regulatory bodies, sponsoring institutions, individual programs, faculty, and academic leaders that together prepare physicians to practice,(5) this issue is much larger than line items in state and federal budgets. However, because of the state’s significant investment in health-related institutions, Texas lawmakers and taxpayers can demand a better return to achieve gains in physician recruitment, education, and training that will benefit the state now and in the future.
Twenty years ago, these issues were pressing. Now, the need for reform is critical as more realize the urgency of the primary care physician workforce shortage and the role academic institutions play in reversing a troubling trend.
“A rational health care system must be based upon an infrastructure consisting of a majority of generalist physicians trained to provide quality primary care and an appropriate mix of other specialists to meet health care needs. … Physicians who are trained, practice, and receive continuing education in the generalist disciplines provide more comprehensive and cost-effective care than nonprimary care specialists and subspecialists.”(3)
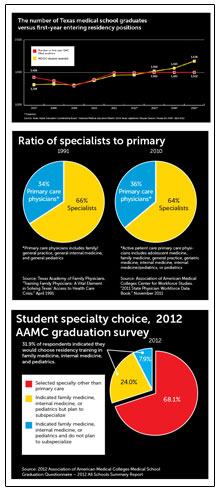
In COGME’s Third Report and TAFP’s “The Right Kind of Doctors for Texas,” the authors challenged institutions to correct the lopsided ratio of specialists to primary care physicians—defined as physicians who practice family medicine, general internal medicine, and general pediatrics—to resemble the 50-50 ratio seen in other developed countries that demonstrate better health outcomes than the United States.(6)
The authors of COGME’s Twentieth Report wrote, “There is significant evidence that optimal health care outcomes and optimal health system efficiency are demonstrated when at least 40-50 percent of the physician workforce is composed of primary care physicians.”
In 2010, the most recent data available, only 36 percent of U.S. doctors were classified as active patient care primary care physicians—or physicians in adolescent medicine, family medicine, general practice, geriatric medicine, internal medicine, internal medicine/pediatrics, or pediatrics. Approximately 35 percent of Texas doctors practiced primary care in 2010.(7)
Already exceeding 26 million, the Texas population is projected to grow steadily to well over 30 million by 2020 and between 35 million and 40 million by 2030. And the number of Texans between age 65 and 74—a segment that demands more complex and coordinated care—is expected to double between 2012 and 2030, from about 1.5 million to 3 million.(8)
Texans already experience lack of access to health care in both rural and urban underserved areas. Nationwide, there were 79.4 primary care physicians in active practice per 100,000 population in 2010, but Texas averaged 62 per 100,000 population.7 Data from the Texas Department of State Health Services show that 29 Texas counties do not have any primary care physicians, 77 counties have fewer than 39.7 primary care physicians per 100,000 population, and 80 counties have fewer than 62.4 primary care physicians per 100,000 population.(9) Three out of every four Texas counties are designated as whole or partial primary care health professional shortage areas, or HPSAs.(9)
Additionally, there are a considerable number of primary care physicians currently practicing who may leave the field as they retire, relocate, enter another specialty, or take an administrative position. Of the 242,500 primary care physicians in the U.S., COGME’s Twentieth Report identified 55,000, or almost one-quarter, as age 56 or older. In Texas, the Texas Higher Education Coordinating Board reports that 45 percent of all physicians are 51 years of age or older and 20 percent are 61 years of age or older. Though physicians tend to retire later than most other professionals, the potential exacerbation of the current shortage is staggering.(10)
At the same time, the pipeline that supplies our future primary care workforce is drying up and stakeholders must act quickly to address this. It takes 11 years to train a new doctor—four years in an undergraduate college setting, four years in medical school, and three years minimum to complete a residency program in a primary care specialty—and student interest in primary care is declining.
“Although the current deficit in the production of primary care physicians is caused by many factors not directly related to the medical education process, medical schools must play a central role in improving preparation and production of students for entry into primary care specialties to meet the nation’s health care needs.”(4)
On the 2012 Association of American Medical Colleges Graduation Questionnaire,(11) a promising 31.9 percent of U.S. medical school graduates indicated that they would choose family medicine, internal medicine, or pediatrics. However, this number is inflated by those in internal medicine or pediatrics who will subspecialize after their first three years of residency. Of the 31.9 percent indicating their interest in primary care, 75.1 percent reported that they plan to go into a subspecialty. Only 24.9 percent of the 31.9 percent said they would not subspecialize.
COGME identifies several reasons for decreased medical student interest in primary care: heavy workload, insufficient reimbursement, a lack of strong primary care role models, and the “hidden curriculum” in medical school. Then, as medical students consider their future practice environment, they see declining reimbursement in primary care relative to specialties, increasing workloads, and increasing administrative burden that continue to erode their interest.(4)
This hidden curriculum is a strong force formerly only spoken about anecdotally as faculty members actively discouraged bright students away from primary care and toward more prestigious subspecialties. As COGME describes it, though, the structure of medical school itself pushes students away from the adult primary care specialties.
“During clinical training, impressionable medical students work shoulder-to-shoulder with residents, interns, and their supervising faculty. This is their first glimpse of the ‘real world’ of medical practice and they are fed a steady diet of subspecialization. This is because most medical schools have, in one form or another, a faculty practice plan anchored to a large hospital that attracts acutely ill patients.
“Furthermore, students receive relatively less exposure to ambulatory practice compared to their inpatient experience. Ambulatory practice is tightly managed and requires a high level of productivity. Placing students in this setting disrupts this productivity and requires financial support to offset this cost. The result is that most medical students have heavy exposure to serious acute subspecialty inpatient care and very little exposure to ambulatory care, where most of American medicine is practiced. The opportunity for exposure to role models in primary care practice is very limited.”(4)
In the 1991 document, TAFP found that the medical reimbursement system favors procedural skills over cognitive skills and, therefore, pays substantially less for the care provided by primary care training programs. As echoed by COGME’s Twentieth Report, the ambulatory settings ideal for primary care training are more costly than inpatient settings and less favorable for medical schools to use to train medical students.
TAFP also found in 1991 that the limited availability of research funds to family medicine means that family medicine departments in medical schools inherently do not generate significant grant dollars; the total amount of external research dollars available for family medicine use is only a fraction of what exists for other subspecialties. The pressure on medical schools to generate revenue makes it difficult to give primary care disciplines equal status because there is not an equal ability for those areas to generate higher income.
Again, COGME’s Twentieth Report demonstrates how little has changed: “Medical school deans and university presidents have traditionally been judged on their ability to build large medical research enterprises focused on discovery and innovation. Most academic medical centers focus on technology-intensive care to pursue these institutional goals, emphasize basic science and clinical investigation, and provide relatively greater rewards to subspecialty care. In most schools, the family medicine department, dedicated to primary care, is dwarfed in size and prestige by the department of internal medicine, which is often the largest research department in the entire university.”
As expenses outpace state support for medical education and the state cuts funds to academic institutions, Texas medical schools have been forced to seek additional funding to supplement their revenue. And as medical schools have increased their dependence on external funding, priorities have shifted. Medical schools understandably tend to favor research and procedural inpatient care—which bring revenue—over the workforce needs of the state.
In the larger sense, medical schools all share a basic purpose—to educate physicians to care for the population. But our medical schools fall short of achieving basic standards shown to improve the health of the community: whether they have produced an adequate number of primary care physicians, ensured adequate distribution of physicians to underserved areas, and added a sufficient number of minority physicians to the workforce. A national report released in 2010 ranked the schools based on these criteria.(12)
Out of the 141 medical schools in the ranking, no Texas schools made the top 50 overall, four ranked in the lowest 40, and one was next to last. In the category of production of primary care physicians, the Texas College of Osteopathic Medicine at the University of North Texas Health Science Center ranked seventh in the nation, but the next Texas school came in at number 40, and three Texas schools ranked in the lowest quarter.(12)
“Ensuring that GME meets the needs of the public will require reevaluation and revision of the present physician payment and GME reimbursement systems, which exert a dominant influence on specialty choices, the types and locations of institutions participating in GME, and the number and specialty mix of GME positions.”(5)
While enrollment in Texas medical schools jumped 31 percent from fall 2002 to fall 2011, increasing from 1,342 students enrolled to 1,762, and with recent campaigns to open at least two new medical schools in south and central Texas, the number of Texas residency positions that could train these newly graduated physicians has remained flat. This creates an economic drain as Texas taxpayers subsidize other states’ workforces.
THECB reports that in fall 2011, the ratio of first-year entering residency positions to graduates was close to 1-to-1, with 1,494 first-year entering residency positions available for the 1,458 medical school graduates. However, with increases in medical school enrollment and stagnation in the number of first-year residency positions, starting in 2014, at least 63 graduates of Texas medical schools will not have an opportunity to enter a Texas residency program. By 2016, at least 180 medical school graduates will have to leave the state for their first year of residency training due to a lack of residency positions.(10)
Because the state invests approximately $168,000 to educate each medical student, failing to add Texas residency positions results in an annual loss of investment in the physician workforce that will reach $30.2 million by 2016.(10) Adding first-year residency positions will reduce the loss of medical school graduates to other states and, eventually, reduce the loss of Texas-trained physicians.
Data from the Association of American Medical Colleges supports this. Though graduates of Texas medical schools or Texas residency programs are not guaranteed to remain in the state once they complete medical training, Texas has one of the highest retention rates of its medical school and residency program graduates in the nation.
Of physicians who complete both undergraduate medical education and graduate medical education in Texas, 80.2 percent stay in Texas, the third best in the nation. Of physicians who only complete undergraduate medical education in Texas, 59 percent stay in Texas, the second highest rate in the country. And of those who only complete graduate medical education in the state, 57.9 percent of physicians stay in Texas, the fifth highest rate in the country.(7)
TAFP asserts that the state must invest in primary care residency positions to have a direct effect on the most dire workforce shortages and counteract the historical movement away from funding primary care residency slots.
From 2000 to 2012, the number of first-year residency positions offered in Texas through the National Residency Matching Program and the American Osteopathic Association Intern/Resident Registration Program increased by 18.6 percent, from 1,281 positions to 1,519 positions. During the same period, the number of family medicine residency positions offered through NRMP in Texas dropped 15 percent, from 247 to 210. The number of family medicine residency positions available today only represents 13.8 percent of training slots offered in the state.
The other primary care residencies have experienced similar declines in Texas. In internal medicine–primary care, the number of residency positions offered in Texas dropped from 445 to 300, a decrease of 33 percent, and the positions offered in internal medicine–pediatrics declined from 392 to 344, or 12 percent. In pediatrics–primary, the number of positions offered dropped from 110 to 64, a decrease of 42 percent.(13)
Nationally, the Macy Foundation found that the number of residents in subspecialty training has risen five times faster than the number of residents in primary care specialties.(5) On the current course, this defies any effort to rebalance the ratio of specialists to primary care physicians.
Part of the decline in positions offered in family medicine residencies can be attributed to shifting priorities in institutions providing graduate medical education, much like the medical schools. Lack of financial support has led to the closing of three family medicine residencies over the past decade, which also results in the loss of related benefits enjoyed by their surrounding communities. Research has shown that the care delivered in primary care clinics operated by family medicine residency programs is better coordinated and more cost-effective. In addition, a significant portion of the care these clinics provide is for Medicaid and CHIP patients, Medicare patients, and the uninsured.(14)
Christus St. Elizabeth Family Practice Residency Program in Beaumont, of which 88 percent of its 74 program graduates practicing in 2005 practiced in health professional shortage areas, closed in 2002. The Texas Tech University Rural Program in Abilene, successful in training physicians for rural practice, closed in 2008. The Kelsey-Seybold Family Medicine Residency Program in Houston, a highly competitive program considered a model for training new physicians in a team-based, multispecialty environment, closed in 2010.(14)
Among the events leading to Kelsey-Seybold’s termination was the decision by its main teaching hospital, St. Luke’s Episcopal Hospital, to reduce by half the funding for stipends paid to family medicine residents. In a January 2010 article in Texas Family Physician, Steve Spann, M.D., senior vice president and dean of clinical affairs at Baylor College of Medicine, said that St. Luke’s “did that unilaterally and despite some pretty strong protest from us, but they felt it was more to their benefit to put those stipends into neurosurgery.”
Patrick Carter, M.D., chair of the clinic’s department of family medicine, said in the article that the Kelsey-Seybold Clinic needed a subsidy from Baylor College of Medicine of between $400,000 and $450,000 to keep the family medicine residency program viable. But BCM couldn’t save the program and it closed. The state appropriated $7.6 million in state GME formula funding to BCM that year for graduate medical education.(15)
Although funding for educating and training a resident comes through various federal and state funding streams and the cost of educating and training a resident far exceeds the amount of funding received by the state(10), the state’s contribution is essential to support the training of primary care physicians in Texas.
“Because GME is a public good and is significantly financed with public dollars, the GME system must be accountable to the needs of the public.”(16)
Legislators must act to influence the trend of declining student interest and bias against primary care specialties in academic institutions to encourage them to refocus their priorities and implement changes in medical education for the good of the public.
For future generations, Texas must ensure that we have an adequate supply of primary care physicians to care for our population, and that medical students and residents receive the right kind of training to provide the coordination and continuity of care needed by patients to receive the right care at the right time at the right cost.
Texas needs doctors to practice in underserved areas and needs the kind of doctors that can provide cost-effective and affordable medical care. Primary care physicians—and family physicians, in particular—are the doctors best trained to provide preventive care and provide a broad range of medical and surgical care.
The state has played a significant role in the education of physicians. It is vitally important that, in the 83rd Legislature and beyond, the state examines its support of medical education and holds the medical schools and teaching hospitals accountable for producing the physician workforce Texas needs. [See TAFP's recommendations for strengthening primary care in the 83rd Texas Legislature.]
Though it’s long past time to act, stakeholders must take steps now to increase the number of primary care physicians and increase access to health care, quality of care, and the overall health of the public.
References
- Hendricks, Sarah; Roland Goertz; and James White. “Training Family Physicians: A Vital Element in Solving Texas’ Access to Health Care Crisis.” Texas Academy of Family Physicians. April 1991.
- White, James; Stacey Vernon; and Troy Alexander. “The Right Kind of Doctors for Texas: A Strategy for Meeting Physician Workforce Needs of Texas.” Texas Academy of Family Physicians. Feb. 1993.
- Council on Graduate Medical Education. “Third Report – Improving Access to Health Care Through Physician Workforce Reform: Directions for the 21st Century.” U.S. Department of Health and Human Services Health Resources and Services Administration. Oct. 1992.
- Council on Graduate Medical Education. “Twentieth Report – Advancing Primary Care.” U.S. Department of Health and Human Services Health Resources and Services Administration. Dec. 2010.
- Weinstein, Debra, chairperson. “Conference Summary – Ensuring an Effective Physician Workforce for the United States: Recommendations for Reforming Graduate Medical Education to Meet the Needs of the Public. The Second of Two Conferences – The Content and Format of GME.” Presented by the Josiah Macy Jr. Foundation in Atlanta, Ga. May 2011.
- Macinko, James; Barbara Starfield; and Leiyu Shi. “The Contribution of Primary Care Systems to Health Outcomes within Organization for Economic Cooperation and Development (OECD) Countries, 1970–1998.” HSR: Health Services Research. June 2003.
- Association of American Medical Colleges Center for Workforce Studies. “2011 State Physician Workforce Data Book.” Nov. 2011.
- Eschbach, Karl. “Demographic Changes in Texas and Healthcare Work Force in Texas.” Presentation. Prepared for Senate Committee on Health and Human Services. 23 Feb. 2010.
- Texas Department of State Health Services Health Professions Resource Center. “Supply Trends Among Licensed Health Professions, Texas, 1980-2011.” Jan. 2012.
- Texas Higher Education Coordinating Board. “Graduate Medical Education Report: 82nd Texas Legislature, Regular Session, House Bill 2908.” April 2012.
- Association of American Medical Colleges. “Medical School Graduation Questionnaire – 2012 All Schools Summary Report.” July 2012.
- Mullan, Fitzhugh, et al. “The Social Mission of Medical Education: Ranking the Schools.” Annals of Internal Medicine, Vol. 152, No. 12. 15 June 2010.
- American Academy of Family Physicians. “2012 Match Summary and Analysis.” Tables 1, 4, 7, 8, and 14. May 2012. Accessed 20 Aug. 2012. http://www.aafp.org/online/en/home/residents/match.html
- Texas Academy of Family Physicians. “Family Medicine Residency Programs Are Critical in Training Texas’ Physician Workforce.” Issue Brief: Improving Texas’ Primary Care Physician Workforce. April 2011.
- Nelson, Jonathan. “On the Brink.” Texas Family Physician, Vol. 61, No. 1, Winter 2010. 21 Jan. 2010.
- Johns, Michael M.E., chair. “Conference Summary – Ensuring an Effective Physician Workforce for America: Recommendations for an Accountable Graduate Medical Education System.” Presented by the Josiah Macy Jr. Foundation in Atlanta, Ga. Oct. 2010.