Primary Care in Texas: Condition Critical
Texas’ primary care workforce shortage threatens the health of the state’s economy and its citizens. The 83rd Texas Legislature can lay the foundation for innovation and improvement in our health care delivery system by reinvesting in our primary care workforce.
By Jonathan Nelson
Long before the U.S. Supreme Court upheld the constitutionality of President Obama’s health care law and lobbed a Medicaid grenade into the political dynamics of state legislatures across the country, Texas lawmakers were already laying the groundwork on a comprehensive strategy to increase the state’s primary care capacity and restore devastating funding cuts in programs designed to produce more primary care physicians.
Notwithstanding what will likely be sharp partisan divisions in how or whether the state implements provisions of the Affordable Care Act, there is a strong consensus among legislative leaders and policy experts across the political and ideological spectrum that Texas must re-examine how the state funds medical education and residency training to ensure we can meet the health care needs of our growing population. With the ACA potentially expanding health insurance coverage to an estimated 5 million currently uninsured Texans starting in 2014, time is of the essence.
“There are compelling economic and demographic realities driving the need to strengthen our primary care workforce that transcend the political volatility of health care,” says TAFP President-elect Troy Fiesinger, M.D. “The time has come to re-examine the state’s investment of taxpayer dollars in medical education and residency training, and to restructure that investment to ensure Texas recruits, educates, and trains the physician workforce Texas communities need.”
Hitting the fiscal cliff
Legislative leaders from both sides of the aisle are acutely aware that we have reached the economic tipping point where health care costs have become a drag on the economy. This unabated increase in costs has forced state and federal lawmakers to spend more on programs like Medicaid and Medicare, leaving less for education, transportation, and other important expenditures.
The projections are bleak. In its 2011 long-term fiscal outlook, the U.S. Government Accountability Office reported that if health care cost trends continue unchecked, by 2020, 89 cents of every dollar of federal revenue will go to pay for Medicare, Medicaid, Social Security, and the net interest payments on the federal debt. With 2.8 million baby boomers becoming eligible for Medicare this year and another 75 million awaiting their turn, there is no question that the rising cost of health care is the most significant contributor to the nation’s long-term deficit.
In Texas the news is similarly sobering. From 2001 to 2011, annual state Medicaid spending more than doubled, from about $6.2 billion to $16.1 billion. Health care now consumes 31 percent of the state budget and that portion is growing.
Spiraling increases in insurance premiums have forced employers to divert revenues away from business expansion and wage increases for employees. From 2000 to 2010, the average premium for family coverage in an employer-sponsored health plan in Texas jumped almost 120 percent, from $6,638 to $14,526.
Faced with such unrelenting cost pressure, employers have shifted a growing share of premium costs to their employees, switched to plans offering smaller benefit packages, or have simply stopped providing coverage altogether. According to the Economic Policy Institute, only 51 percent of non-elderly Texans were covered by employer-sponsored plans in 2009 and 2010, down from 61 percent just a decade earlier. A 2012 Rand Corporation report found these increases have wiped out a decade of income gains for the average American family. The fiscal burdens imposed on federal and state budgets, employers, and families by rising health care costs can no longer be ignored.
The primary care conundrum
The health care cost crisis is inescapably linked to the way in which medical services are delivered and financed. Despite substantial evidence that when patients have adequate access to primary care physicians, communities enjoy improved health care outcomes, better overall health, and lower health costs, Texas suffers from a shortage of primary care physicians. Political and budgetary decisions have stalled system-wide improvements to transform our fragmented health care delivery system into one that supports high-quality, cost-efficient, and well-coordinated primary care.
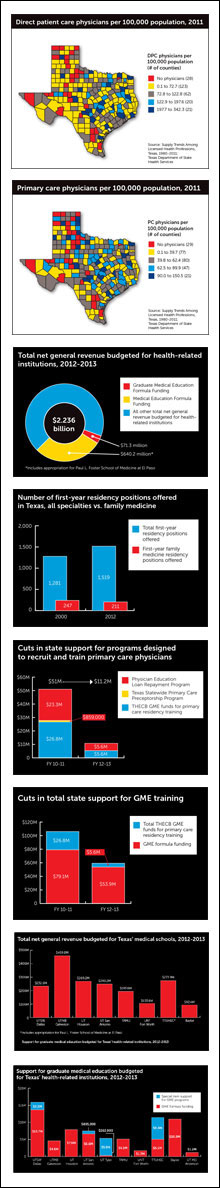
Nearly 20 years ago, the Council on Graduate Medical Education issued a blistering report warning policymakers that our nation had too few primary care physicians. Little has changed since. Approximately 18,000 primary care physicians practice in Texas, serving a population that will soon exceed 26 million. This ratio falls far below the national average and will worsen as Texas’ population continues to balloon at both ends of the age spectrum. Compounding the problem is the poor distribution of primary care physicians throughout the state. Three of every four Texas counties are designated as whole or partial Primary Care Health Professional Shortage Areas.
Many factors contribute to Texas’ inability to produce and sustain an adequate primary care physician workforce. Long work hours, huge patient loads, and a growing income gap between primary care physicians and specialists discourage medical students from pursuing careers in primary care. Add to that the rising expense of medical education, which saddles graduates with an average of more than $150,000 in debt, and it’s perfectly rational that so few medical students choose primary care.
But there are other influences at play, and to understand them, you have to know a bit about how residency training is financed. The majority of graduate medical education funding comes from the Centers for Medicare and Medicaid Services in the form of direct GME payments—intended to reimburse teaching hospitals for the direct cost of training residents including resident stipends and faculty salaries—and indirect medical education payments—intended to pay for the higher cost of patient care at teaching hospitals. Funding amounts for both methods are calculated based on the number of residents in training at a hospital.
Two fundamental problems with Medicare GME funding combine to jeopardize many primary care residency programs, especially family medicine programs. First, Congress capped Medicare GME funding as part of the Balanced Budget Act of 1997. With few exceptions, a teaching hospital can only receive Medicare GME funding for the number of residents it trained in 1996, and while many teaching hospitals have exceeded that cap, they have done so at their own expense.
The other problem is that Medicare only reimburses teaching hospitals for the time residents spend in the hospital, which is fine for most specialties, but detrimental to primary care. For family medicine residents, the majority of training takes place in an outpatient clinic.
Increases in residency training positions since Medicare capped GME funding have occurred almost exclusively in subspecialty training. The Medicare Payment Advisory Committee, COGME, and numerous researchers have observed that teaching hospitals and academic health centers have built GME training programs that serve their institutional goals instead of serving the physician workforce needs of their communities.
Left to their own devices, academic medical centers have little incentive to increase primary care residency training positions. Residents in training provide inexpensive labor for treating patients, so teaching hospitals naturally realize higher revenues when employing residents in procedural specialties compared to residents training in primary care. Robust specialty residencies also present academic medical institutions greater opportunities to receive substantial research grants. Studies have shown there is an inverse proportion between the amount of research grant funding an institution receives from the National Institutes of Health and the number of primary care physicians the institution produces.
Together, these factors set the stage for what COGME calls the “hidden curriculum” medical students encounter at academic health centers. Consider this statement from COGME’s 20th Report: Advancing Primary Care, from 2010:
“Medical school deans and university presidents have traditionally been judged on their ability to build large medical research enterprises focused on discovery and innovation. Most academic medical centers focus on technology-intensive care to pursue these institutional goals, emphasize basic science and clinical investigation, and provide relatively greater rewards to subspecialty care. In most schools, the family medicine department, dedicated to primary care, is dwarfed in size and prestige by the department of internal medicine, which is often the largest research department in the entire university. In addition, many large hospitals have developed GME programs to support their complex care programs. The GME programs of these large teaching hospitals are effective for the recruitment of physicians to the medical staff and for building subspecialty clinical care. This disconnect between meeting the needs of the population versus meeting the needs of the academic health center was the focus of an Institute of Medicine report in 1989 and has recently been an area of concern for the Medicare Payment Advisory Committee.
“Although Medicare capped its funded GME slots in 1997, accredited GME positions have grown 6.3 percent from 2003-2006, virtually all of which are self-funded by the hospitals. Despite this increase, a rise in subspecialty rates led to fewer physicians pursuing generalist careers. Like student choices, this build-out of residency training positions is highly correlated with specialty income. Teaching hospitals invest in lucrative services in order to support their bottom line and residents and fellows are an inexpensive way to support those services. Increasing options for subspecialization has both direct and indirect effects on primary care production, first by closing primary care positions to be used for subspecialty training, and second by giving would-be primary care physicians options to subspecialize. The net effect is a substantial reduction in primary care production from GME, now at about 29 percent or less compared to 32 percent from 2003 to 2008. In bending GME to service their financial bottom line, the needs of the population are not best served.”
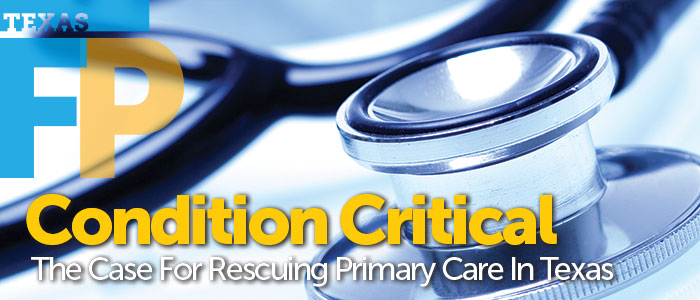
From 2000 to 2012, the number of first-year residency positions offered in Texas through the National Residency Matching Program and the American Osteopathic Association Intern/Resident Registration Program increased by 18.6 percent, from 1,281 positions to 1,519. Over that same period, the number of first-year family medicine residency positions in Texas fell by 14.6 percent, from 247 to 211.
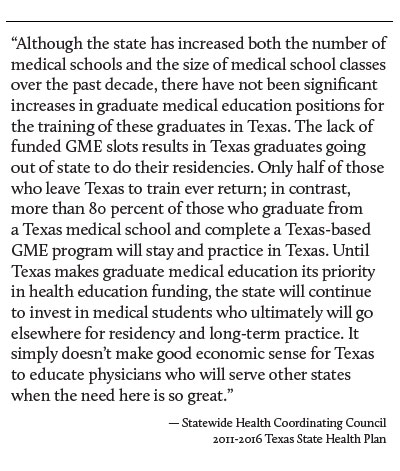
To make matters worse, Texas will soon be graduating more medical students than the number of first-year residency training positions available in the state. A recent report by the Texas Higher Education Coordinating Board shows that from fall 2002 to fall 2011, enrollment in Texas medical schools jumped by 31 percent, from 1,342 to 1,762. Since residency positions have increased more slowly, the coordinating board predicts that without investment in new residency positions for first-year residents, by 2014 Texas medical schools will produce 63 more graduates than the number of first-year positions available. By 2016, the number rises to 180.
According to the medical student funding formula used in the state’s current budget, Texas invests approximately $168,000 to educate each medical student. That’s down from about $200,000 just a couple of years ago. Even if every graduate of a Texas medical school wanted to complete residency training in this state, Texans would still be exporting those who couldn’t find a place to train, thereby subsidizing the physician workforce of other states when the need in Texas is so critical.
Aligning incentives to increase primary care production
In the current fiscal biennium, Texas will spend $2.24 billion in total net general revenue on its 10 health-related institutions in large part for the recruitment, education, and training of its future physician workforce. Yet the state has no reliable way to influence what kind of physicians are produced for that investment or to hold medical schools accountable for producing an appropriate physician workforce to meet the needs of its population. As a result, Texas has developed an imbalanced workforce with too few primary care physicians.
A 2010 study in the Annals of Internal Medicine confirmed as much. The study examined a cohort of graduates from the nation’s 141 allopathic and osteopathic medical schools to rank the schools on their performance in addressing three interrelated shortcomings in the U.S. physician workforce: the insufficient number of primary care physicians, the geographic maldistribution of physicians, and the lack of racial and ethnic diversity among physicians. The authors found that no Texas medical school appeared in the top 50, four ranked in the lowest 40, and one was next to last.
For the production of primary care physicians, the Texas College of Osteopathic Medicine at the University of North Texas Health Science Center ranked seventh in the nation. The next Texas school on the list came in at number 40, and three Texas schools were in the lowest quarter of the rankings.
The amount of state support Texas’ health-related institutions receive will always seem small compared to the net revenues of their affiliated practice plans, research funding, and other sources of revenue. Still state support is significant, and given the state’s desperate need to gain more primary care physicians for the sake of its citizens, its economy, and for the hope of controlling escalating health care costs, medical schools should be expected to produce an appropriate mix of specialist and primary care physicians. Of course medical schools can’t force medical students to pursue primary care careers, but the state could implement incentives to encourage schools to counteract the “hidden curriculum.”
In the upcoming legislative session, TAFP will propose a series of incentives and related structural reforms intended to facilitate a more rational and predictable physician workforce. Those policy reforms are common sense, straightforward, and evidence-based. They have been vetted by Texas’ top policy experts, medical educators, business leaders, and a wide range of health professionals.
First, the Legislature will be urged to increase the number of primary care physicians practicing in Texas by restoring funding to family medicine and primary care residency training programs, and by creating incentives for the development of new training programs based in community clinics, such as federally qualified health centers. Next, lawmakers should target the state’s investment in medical education to get a better return by creating incentives for medical schools to produce the primary care physician workforce Texas demonstrably and urgently needs. Finally, the state can recruit primary care physicians to practice in underserved communities by recommitting to the promise of physician education loan repayment.
“Together, these initiatives constitute a bold set of strategies to grow and improve Texas’ primary care physician workforce and to increase access to primary care services for Texans across the state,” Fiesinger says. “With a robust primary care physician workforce, we can ensure Texas’ patients will receive the right care at the right time for the right price.”
Fast facts
Texas health rankings
When compared with other states, Texas ranks near the bottom in many determinants of health—from behaviors and community factors to public policies and clinical care—which are reflected in poor health outcomes. Consider these 2011 rankings:
| DETERMINANT | RANKING |
| Obesity (percent of adult population) | 42 |
| Lack of health insurance (percent without health insurance) | 50 |
| Early prenatal care (percent with visit during the first trimester) | 50 |
| Primary care physicians (per 100,000 population) | 42 |
| Preventable hospitalizations (number per 1,000 Medicare enrollees) | 36 |
| Diabetes (percent of adult population) | 34 |
| Cardiovascular deaths | 30 |
Source: America’s Health Rankings 2011, United Health Foundation
The economic impact of chronic disease
Experts predict that the combined effect of treatment costs and lost productivity from chronic disease will cost the Texas economy $187 billion in 2013. This figure balloons to $332 billion by 2023.
Source: An Unhealthy America: The Economic Burden of Chronic Disease, Milken Institute, October 2007
The primary care solution
The addition of primary care physicians in a population results in better overall health outcomes for all patients.
- An increase of one primary care physician per 10,000 population (about a 20 percent increase) was associated with a 6 percent decrease in all-cause mortality and about a 3 percent decrease in infant, low-birth-weight, and stroke mortality.
- For total mortality, an increase of one primary care physician per 10,000 population was associated with a reduction of 34.6 deaths per 100,000 population at the state level.
- Lower primary care physician supply and higher specialty-to-population ratios were associated with higher overall age-adjusted mortality, mortality from heart disease, mortality from cancer, neonatal mortality, life span, and low-birth-weight ratios.
Source: Starfield, Barbara, et al. “The Effects of Specialist Supply on Populations’ Health: Assessing the Evidence.” Health Affairs Web exclusive w5.97 (15 March 2005): 97-107.