AAFP leaders advocate for improved access to primary care and more this month on Capitol Hill
By AAFP’s Federal Advocacy Team
On October 12, AAFP’s president, president-elect, and board chair traveled to Washington D.C., to meet with members of Congress and their staff to advocate for key AAFP legislative priorities. Here’s what they discussed:
Stop Medicare payment cuts
- AAFP leadership urged Congressional members to act before the end of this year to stop impending Medicare payment cuts and work toward long-term solutions for sustainable physician payment.
- They pressed support for the bipartisan Supporting Medicare Providers Act of 2022 (H.R. 8800) to offset the 4.5% cut to the Medicare conversion factor for 2023 and enact a positive annual payment update based on the Medicare Economic Index to account for increased physician practice costs and inflation.
- See also: The AAFP and more than 100 other health groups are urging Congress to enact meaningful reforms to stabilize Medicare physician payment and protect beneficiaries’ access to care.
Prior authorization reform
- AAFP leadership thanked House members for passing the Improving Seniors’ Timely Access to Care Act (H.R. 3173/S. 3018), which would reduce administrative tasks that interfere with and delay patient care by streamlining prior authorization in Medicare Advantage plans. They encouraged the Senate to swiftly pass this important legislation before the end of this year to ensure seniors in Medicare Advantage plans have timely, equitable access to care.
Child and adolescent health groups sound the alarm on mental health crisis
Why it matters:
Last October, the AAFP joined the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association in declaring children’s mental health a national emergency. One year later, the AAFP and our partners are calling for further legislative action to address this crisis.
Family physicians and their primary care colleagues play a critical role in identifying mental health conditions, ensuring equitable access to mental health care, and reducing the stigma of mental illness. Without family physicians, the nearly one in five U.S. adults who experience some form of mental illness each year may go untreated.
What we’re working on:
- The AAFP, along with the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association sent a letter to President Biden urging his administration to continue the work to address the youth mental health crisis.
- The AAFP is advocating for the Senate to pass the bipartisan Improving Access to Behavioral Health Integration Act (S. 4306), which would establish a federal grant program for primary care practices to implement evidence-based behavioral health integration programs.
Conrad 30 Program essential to strengthen primary care workforce
Why it matters:
The Conrad 30 Waiver Program allows foreign physicians trained in the U.S. to remain in the U.S. without having to return home if they agree to practice in an underserved area for three years. Many communities, including rural and low-income areas, have problems meeting their patient care needs and depend on the physicians in this program to provide health care services.
The Conrad 30 program was temporarily extended through December 16, 2022, as part of the most recent continuing resolution, but additional action is needed to maintain and expand the program.
With communities across the country facing physician shortages, the Conrad 30 Waiver Program ensures that international physicians who want to continue practicing in the U.S. can continue to provide care for patients during the COVID-19 crisis and beyond.
What we’re working on:
- Last month the AAFP shared with the Senate Judiciary Committee the important role international medical graduates play in addressing physician shortages, especially in rural and medically underserved areas.
- We urge Congress to pass the Conrad State 30 and Physician Access Act (S.1810/H.R. 3541) as well as the Health Care Workforce Resilience Act (S. 1024) to increase access to care in medically underserved communities and to strengthen the primary care workforce.
AAFP urges HHS to delay information blocking deadline
Why it matters:
AAFP told HHS that family physicians and most other stakeholders need more time and improved guidance to ensure compliance with electronic health information sharing rules. This includes a broad and potentially burdensome expansion of how EHI is defined.
Family physicians need accessible, actionable patient health information at the point of care, which is why the AAFP has long advocated to advance interoperability. However, without improved data sharing functionality, we’re concerned this latest implementation deadline could lead to more administrative burden.
What we’re working on:
- The AAFP urged HHS to postpone the deadline by one year and cautioned against imposing financial penalties on clinicians without first providing them the opportunity to correct any violations.
- We are advocating to improve health data sharing and patient access to their electronic health information without increasing administrative workload for physicians or compromising data privacy.
AAFP submits comments on nondiscrimination rule
The AAFP submitted comments to HHS in response to their Nondiscrimination in Health Programs and Activities proposed rule. Family physicians know that access to inclusive, person-centered care improves health outcomes.
The AAFP urged HHS to strengthen non-discrimination protections in all health settings and programs including medical services, insurance coverage, and benefit design. The AAFP also weighed in on new provisions to address discriminatory clinical algorithms and urged HHS to ensure new health IT or translation requirements under this rule are accessible and financially feasible for all practices, especially small and solo physician practices.
Family physicians provide majority of obstetric care in maternity care deserts
New research from the Robert Graham Center show in many maternity care deserts, family physicians are the sole maternity care clinicians. The data demonstrate the significant role family physicians play in MCDs and nationwide.
Key findings include:
- Family physicians deliver babies in more than four in 10 (40.7%) of all U.S. counties, and more than five in 10 (52.4%) of these counties are located in nonmetropolitan areas.
- Family physicians are the sole maternity care clinicians delivering babies in 181 maternity care deserts (about one in six of all MCDs), serving more than 400,000 women.
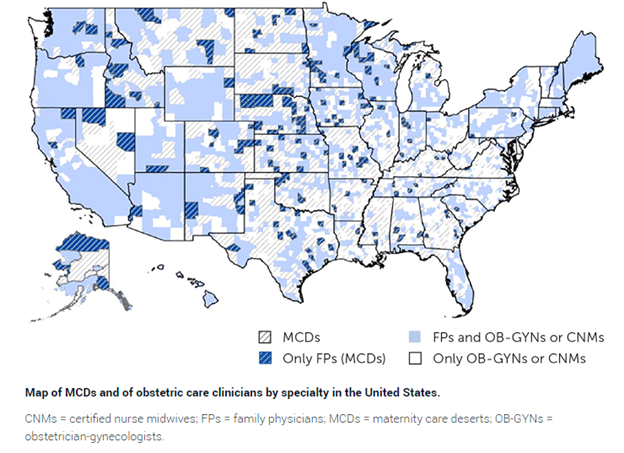
Sources: American Board of Family Medicine, 2011–2019; Area Health Resource File, 2021
For the latest policy updates impacting family medicine, follow us at @aafp_advocacy.