Budget slashes 80 percent of support for programs designed to increase primary care physician workforce
Budget slashes 80 percent of support for programs designed to increase primary care physician workforce
By Jonathan Nelson
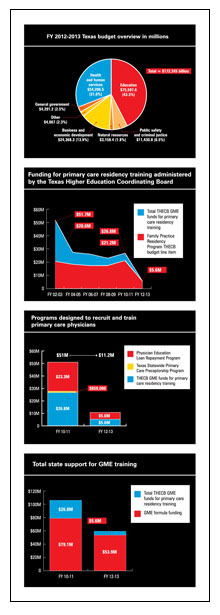
As lawmakers crafted and passed innovative, market-based health delivery system reforms designed to increase clinical integration, care coordination, and disease management, all the while touting the cost-saving and quality-improving benefits of primary care, the Legislature slashed total state support for graduate medical education by almost 40 percent.
Lawmakers reserved the most drastic cuts for a set of programs administered by the Texas Higher Education Coordinating Board specifically designed to support the recruitment and residency training of family physicians and other primary care physicians, and to encourage them to practice in underserved communities throughout the state. The Legislature cut the line item supporting family medicine residency programs by 73.6 percent, going from $21.2 million in the current biennium to $5.6 million in the next. Two other line items for residency training were eliminated, as was all funding for the Statewide Primary Care Preceptorship Program.
Finally, the state’s new Physician Education Loan Repayment Program, created by the last Legislature, was cut from $23.2 million in 2010-2011 to $5.6 million in 2012-2013. According to analysis by the Texas Primary Care Office at the Department of State Health Services, this reduction could affect health care access for 1.1 million Texans in underserved areas.
Altogether, the budget decisions for these programs constitute a withdrawal of $39.8 million, or 80 percent, in the state’s investment in the production of its primary care workforce.
“I think it’s tragically shortsighted,” says TAFP member Dana Sprute, M.D., M.P.H., residency program director at the University of Texas Southwestern—Austin Family Medicine Program. “At a time when we should be advocating for not just supporting what we already are doing but expanding the number of primary care GME slots, we’ve actually cut it.”
Sprute says the state already doesn’t have enough residency training positions to produce enough primary care physicians to care for Texas’ growing population. “By defunding GME slots, and primary care specifically, they’ve made this circumstance worse. We’ll have an even further brain drain out of our state where we pay to educate medical students only to send them out to other states for residency training because we haven’t been able to meet the need for expanded GME slots. In fact, this will have the effect of contracting them, I’m sure.”
TAFP CEO Tom Banning expressed similar sentiments to the Texas Tribune in June, adding that the cuts would likely lead to the closure of some of the state’s 28 family medicine residency programs. “We’ve already seen two family medicine programs close over the last four years. We will have fewer physicians caring for Texas patients at a time we need to be growing that physician base.”
In a survey of family medicine residency programs receiving funds through the THECB, seven programs reported their existence would be threatened if the coordinating board funding were eliminated.
The severe reduction will spell the end of the Family Practice Faculty Development Center, which has been training faculty for family medicine residency programs since 1978. Located in Waco, the center receives the majority of its funds from the THECB through the Family Practice Residency Program budgetary line item.
The coordinating board uses another portion of those funds to support rural and public health rotations, through which residents experience one-month rotations in practices serving communities in need. The Legislature established the rural rotation program in 1989 to increase access to family medicine in underserved communities, and it has had measurable success. In the last 15 years, about 82 family medicine residents on average have participated in the program each year. Approximately 15 percent of the program’s participants since 1991 are practicing today in a rural community in Texas, with 14 percent serving in counties with less than 50,000 people.
For the next two years, there will only be enough funds for about 20 residents to participate in the rural rotations. Sprute says her program has required all residents to complete rural rotations for years and that many have gone on to practice in underserved communities. “We’re not able to send people to the rural rotation anymore because we don’t have the ability to pay for it,” she says. “So fewer residents will be exposed to rural medicine, making worse the health professional shortage areas that we have.”
The Legislature directed the THECB to conduct an interim study on the adequacy of the state’s GME capacity to produce an appropriate number of physicians of each specialty. That should be an interesting study, to say the least.