Changes in complexity of ambulatory care from 2005 to 2008 across disciplines
Changes in complexity of ambulatory care from 2005 to 2008 across disciplines
By David A. Katerndahl, M.D., M.A.; Robert Wood, Dr. P.H., Carlos R. Jaén, M.D., Ph.D.
Between 1996 and 2001, more primary care physicians perceived that the complexity of care they provided was increasing (from 32 percent of physicians in 1996-1997 to 36 percent physicians in 2000-2001) according to the Community Tracking Survey (Kemper et al., 1996; Metcalf et al., 1996). In addition, 26 percent of physicians believed that the complexity of care they were expected to provide was greater than it should be.
Such increasing complexity could have several ramifications. First, as systems become more complex, the rate of errors rises (Bar-Yam, 1997). The risk of errors increases with incomplete knowledge, seeing multiple patients, use of multiple medications, and implementation of complex procedures (Croskerry et al., 2004). These conditions seem to describe primary care and may explain why errors were found to occur in 24 percent of family medicine office visits (Elder et al., 2004). This is consistent with error reduction strategies which advocate ways that reduce unnecessary complexity, such as standardizing approaches, bundling related tasks, and using pre-existing habits (Elgert, 2005). A second potential impact would be a decline in perceived autonomy and ultimately career satisfaction among primary care physicians (Katerndahl et al., 2009). In a recent physician survey, only 31 percent of physicians felt that their autonomy met or exceeded their expectations (Hadley et al., 1999) and perceptions of autonomy are generally poorer among primary care than specialty care physicians (Burdi and Baker, 1999). Similarly, between 1991 and 1996, the proportion of physicians who indicate that they are very satisfied with their careers dropped from 48 percent to 37 percent (Burdi and Baker, 1999) while a survey published in 1999 put that figure at 33 percent (Hadley et al., 1999). Although there is no evidence that these declines are due to an increase in perceived complexity, the trends are consistent with that explanation. Thirdly, in an attempt to cope with perceived complexity, one approach would be to lower the threshold at which patients are referred to specialists. In fact, one study found that the referral rate from primary care physicians more than doubled between 1978 and 1994 (Stafford et al., 1999). A final potential consequence of increased complexity of care is a reduction in the overall quality of care provided (St. Peter et al., 1999). This may explain why only 55 percent of adult patients received recommended care (McGlynn et al., 2003). Poor quality of care was especially noted in time-intensive activities, such as history-taking, counseling, and patient education (McGlynn et al., 2003) as well as screening and preventive medicine (Asch et al., 2006). By the increasing perceived complexity, there are trends suggesting a decrease in the services provided by primary care physicians (Mechanic et al., 2001; Safran, 2003).
Comparison studies suggest that the quality of care provided for specific medical conditions is “poorer” in primary care than in specialty settings. For example, family physicians more often recommend therapies which are less beneficial for acute myocardial infarction than do cardiologists (Ayanian et al., 1994). In addition, cardiologists are less likely to order tests but prescribe more medications for hypertension and ischemic heart disease (Greenwald et al., 1984). Cardiologists also perform more cardiac catheterizations in patients with heart failure (Philbin and Jenkins, 2000). Similar differences between family physicians and psychiatrists have been reported in patients with mental disorders. Studies suggest that, compared with psychiatrists, primary care physicians more often fail to detect mental disorders (Thompson et al., 2001; Rost et al., 1998; Simon et al., 1999), make more diagnostic errors (Ryan, 1994; Hoffman, 1982), and more often use inappropriate or inadequate dosages of psychotropic medications (Katon et al., 1995; Olfson and Klerman, 1993).
Using a recently developed approach for estimating relative complexity of ambulatory care, Katerndahl et al. (2011) found that there was minimal difference in the unadjusted input and total encounter complexity of general/family practice and cardiology in 2000; psychiatry’s input was less complex. Cardiology encounters involved more input quantitatively, but the diversity of general/family practice input eliminated the difference. Cardiology also involved more complex output. However, when the duration of visit was factored in, the complexity of care provided per hour in general/family practice was 33 percent more relative to cardiology and five times more relative to psychiatry.
The purpose of this study was to estimate changes in the complexity of patient encounters in three disciplines (family medicine, cardiology, and psychiatry) using data from two years of the National Ambulatory Medical Care Survey.
Methods
In a prior study funded through the Texas Academy of Family Physicians Foundation (Katerndahl et al., 2010), we developed and evaluated a method for estimating relative complexity based upon the quantity, diversity, and variability of clinical encounters, derived from national databases. In this study, we used this method to analyze data from two years of the NAMCS databases (NCHS, 2005; NCHS, 2008) for family practice, cardiology, and psychiatry; the 2005 and 2008 databases were used because the data fields were quite similar for years 2005-2008.
Computation of Complexity of Each Input/Output. The complexity of each input/output is defined as the mean input/output per clinical encounter weighted by its inter-encounter diversity and variability. Thus, the complexity of diagnoses seen in family practice would be the product of the mean number of diagnoses seen in family practice encounters (1.75 diagnoses using the 2000 NAMCS data), the inter-encounter diversity of diagnoses weighting, and the inter-encounter variability of diagnoses weighting. The diversity of an input/output is defined as the proportion of the number of categories needed to include 95 percent of the input/output reported out of the total possible categories. The 95-percent proportion was chosen to minimize the impact of a rare or miscoded input/output. The variability was defined as the coefficient of variation (COV) of the input/output, which is calculated as the standard deviation divided by the mean. The COV was chosen over other measures of variation because it is a unit-free measure (Armitage and Berry, 1987). To standardize the weightings and limit the impact of low diversity or variability on complexity, the weightings used are the Z-transformations of the diversity proportion and the COV, and range between 0.5 and 1.0.
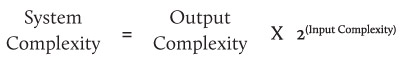
Computation of Total Complexity. Once the complexity of each component has been calculated, the total input and total output complexities are calculated by summing the component complexities (Bar-Yam, 1997). However, calculation of the total specialty complexity is not merely the sum of the input and output complexities. A fundamental principle of complex systems is that there is a logarithmic relationship between input and output, so that, as the information in the input increases linearly, the complexity of the system increases exponentially. Thus, for binary data, the total system complexity is determined by the following formula (Bar-Yam, 1997):
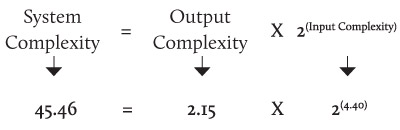
In the complexity of family practice using the 2000 NAMCS data, the total input complexity is the sum of the complexities of reasons-for-visit (0.78), diagnoses (0.82), examination/testing (0.83), and patient characteristics (1.97). Using the formula presented above, we calculate the total specialty complexity as:
Finally, we can determine confidence intervals around estimates using bootstrap methods.
If we are to assess the impact of the complexity of the encounter on the physician, we need to adjust the estimated complexity for the duration of visit. Temte et al. (2007) have suggested the encounter problem density (number of clinical problems addressed per hour) as a measure of complexity. Although simpler to measure, such assessments do not address the diversity and variability of patients and problems, which also contribute to the mental burden to the physician. For our purposes, the estimated complexity is divided by the duration of visit to obtain the complexity per minute. An hourly complexity density estimate (Temte et al., 2007) is derived by multiplying the complexity per minute by 60. The complexity density represents the complexity burden on the physician.
Results
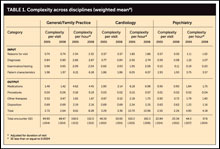
Table 1 presents the final results of this analysis. In all cases, family medicine and cardiology provided significantly more complex care than did psychiatry. From 2005 to 2008, the complexity of ambulatory care provided by family physicians and psychiatrists declined slightly due primarily to a decrease medication and non-medication therapies; overall, care in family medicine visits was more than twice as complex as in psychiatric visits. However, the complexity of ambulatory cardiology care rose with increases in both input and output complexity primarily due to increased complexity of diagnoses and medications.
In addition, complexity density also declined for both family medicine and psychiatry due primarily to increases in the mean durations of visit for both disciplines from 18.95 to 19.13 minutes in family medicine and from 30.90 to 32.47 minutes in psychiatry. Cardiology, however, reported a slight decline in mean duration of visit from 18.45 to 18.39 minutes between 2005 and 2008 with a resulting increase in input and output complexity densities. While family medicine had the most overall complexity density in 2005 (158) compared with cardiology (150), by 2008, that of cardiology had surpassed family medicine (165 versus 152).
Discussion
Changes in complexity of visits and complexity density for disciplines may have important implications. First, complex systems generate errors in proportion to the level of complexity of the system (Bar-Yam, 1997). Thus, we should anticipate that the risk of medical errors may be increasing for cardiology but declining in family medicine. Second, because perceived complexity correlates with perceived clinical autonomy and career satisfaction (Katerndahl et al., 2009), these observed changes may represent good news for family medicine but a warning for cardiology. Finally, the continuing mismatch between complexity of care provided and levels of reimbursement must be addressed.
References
- Armitage P, Berry G: Statistical Methods In Medical Research (2nd ed). Boston: Blackwell Scientific Publications, 1987.
- Asch SM, Kerr EA, Keesey J, Adams JL, Setodji CM, Malik S, McGlynn EA: Who is at greatest risk for receiving poor quality of health care? N Engl J Med 2006; 354:1147-56.
- Ayanian JZ, Hauptman PJ, Guadagnoli E, Antman EM, Pashos CL, McNeil BJ: Knowledge and practices of generalist and specialist physicians regarding drug therapy for acute myocardial infarction. N Engl J Med 1994; 331:1136-42.
- Bar-Yam Y: Dynamics of Complex Systems. Reading, MA: Perseus Books, 1997.
- Burdi MD, Baker LC: Physicians’ perceptions of autonomy and satisfaction in California. Health Affairs 1999; 18:134-45.
- Croskerry P, Shapiro M, Campbell S, LeBlanc C, Sinclair D, Wren P, Marcoux M: Profiles in patient safety. Acad Emerg Med 2004; 11:289-99.
- Elder NC, Vander Meulen MB, Cassedy A: Identification of medical errors by family physicians during outpatient visits. Ann Fam Med 2004; 2:125-9.
- Elgert S: Reliability science. Fam Pract Mgmt 2005; October issue:59-63.
- Greenwald HP, Peterson ML, Garrison LP, Hart LG, Moscovice IS, Hall TL, Perrin EB: Interspecialty variation in office-based care. Med Care 1984; 22:14-29.
- Hadley J, Mitchell JM, Sulmasy DP, Bloche MG: Perceived financial incentives, HMO market penetration, and physicians’ practice styles and satisfaction. HSR 1999; 34:307-21.
- Hoffman RS: Diagnostic errors in the evaluation of behavioral disorders. JAMA 1982; 248:964-7.
- Katerndahl DA, Parchman M, Wood R: Perceived complexity of care, perceived autonomy, and career satisfaction among primary care physicians Journal of the American Board of Family Medicine 2009; 22:24-33.
- Katerndahl DA, Wood R, Jaén CR. A method for estimating relative complexity of ambulatory care. Annals of Family Medicine 2010; 8:341-347.
- Katerndahl DA, Wood R, Jaén CR. Family medicine outpatient encounters are more complex than those of cardiology and psychiatry. Journal of the American Board of Family Medicine 2011; 24:6-15.
- Katon W, Von Korff M, Lin E, Walker E, Simon GE, Bush T, Robinson P, Russo J: Collaborative management to achieve treatment guidelines. JAMA 1995; 273:1026-31.
- Kemper P, Blumenthal D, Corrigan JM, et al.: Design of the Community Tracking Study. Inquiry 1996; 33:195-206.
- McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA: Quality of health care delivered to adults in the United States. N Engl J Med 2003; 348:2635-45.
- Mechanic D, McAlpine DD, Rosenthal M: Are patients’ office visits with physicians getting shorter? N Engl J Med 2001; 344:198-204.
- Metcalf CE, Kemper P, Kohn LT, Pickreign JD: Site definition and sample design for the Community Tracking Study. Washington, DC: Center for Studying Health System Change, 1996.
- National Center for Health Statistics. National Ambulatory Medical Care Survey. Hyattsville, MD: U.S. Department of Health and Human Services, 2005 and 2008.
- Olfson M, Klerman GL: Trends in the prescription of psychotropic medications. Med Care 1993; 31:559-64.
- Philbin EF, Jenkins PL: Differences between patients with heart failure treated by cardiologists, internists, family physicians, and other physicians. Am Heart J 2000; 139:491-6.
- Rost K, Zhang M, Fortney J, Smith J, Coyne J, Smith GR Jr: Persistently poor outcomes of undetected major depression in primary care. Gen Hosp Psychiatry 1998; 20:12-20.
- Ryan DH: Misdiagnosis in dementia. Intl J Geriatr Psychiatry 1994; 9:141-7.
- Safran DG: Defining the future of primary care. Ann Intern Med 2003; 138:248-55.
- Simon GE, Goldberg D, Tiemens BG, Ustun TB: Outcomes of recognized and unrecognized depression in an international primary care study. Gen Hosp Psychiatry 1999; 21:97-105.
- St. Peter RF, Reed MC, Kemper P, Blumenthal D: Changes in the scope of care provided by primary care physicians. N Engl J Med 1999; 341:1980-5.
- Stafford RS, Saglam D, Cuasino N, Starfield B, Culpepper L, Marder WD, Blumenthal D: Trends in adult visits to primary care physicians in the United States. Arch Fam Med 1999; 8:26-32.
- Temte J, Grasmi9ck M, Barr J, Kunstman J, Jaeger A, Beasley J: Encounter problem density in primary care: a better measure of complexity? Presented at the annual meeting of the North American Primary Care Research Group on October 20-23, 2007 in Vancouver, British Columbia.
- Thompson C, Ostler K, Peveler RC, Baker N, Kinmonth AL: Dimensional perspective on the recognition of depressive symptoms in primary care. Br J Psychiatry 2001; 179:317-23.
Support for TAFP Foundation Research is made possible by the Family Medicine Research Champions.
Gold level
Richard Garrison, M.D. David A. Katerndahl, M.D.Jim and Karen White
Bronze level
Joane Baumer, M.D. Carol and Dale Moquist, M.D. Lloyd Van Winkle, M.D.George Zenner, M.D.
Thank you to all who have donated to an endowment. For information on donating or creating a new endowment or applying for research grants, contact Kathy McCarthy at kmccarthy@tafp.org.
 Click to view chart.
Click to view chart.