A small investment for a large return: The Texas Statewide Preceptorship Program
A small investment for a large return:
The Texas Statewide Preceptorship Program
By Kate McCann
With federal health care reform expanding insurance coverage to an estimated 4.2 million Texans over the next four years and a dwindling pipeline of primary care physicians to care for this newly insured population, increasing the number of medical students choosing careers in primary care must be one of the state’s top priorities.
One initiative, the Texas Statewide Preceptorship Program, makes a quiet but significant impact on student specialty choice for a relatively small investment of state funds. Plus, the turnaround for a medical student from preceptorship to primary care practice can be as short as five years. As the 82nd Texas Legislature convenes in January 2011 and the state faces a multibillion dollar shortfall, proponents of the program encourage state leaders to take a careful look before sending the preceptorships back to the chopping block.
The Texas Statewide Preceptorship Program provides funding to first- and second-year medical students to spend up to four weeks in a primary care physician’s office experiencing the daily life and work of doctors in the specialties of family medicine, general internal medicine, or general pediatrics. Because many of these pre-clinical students have never experienced medicine outside of the academic setting, daily tasks mostly include observation, taking patient histories, learning to formulate treatment plans, identifying early diagnoses for common disorders, and polishing presentation skills.
More than witnessing the daily routine of their volunteer physician preceptor, the students gain one-on-one mentorship and a glimpse of “real-world medicine.” Many leave their preceptorship with a very different idea of primary care.
This was the case with Travis Bias, D.O., currently a third-year family medicine resident and co-chief of his residency class at Memorial Family Medicine Residency Program in Houston. He entered medical school wanting to become an orthopedic surgeon, dismissing family medicine as monotonous and boring. He was also concerned about repaying his medical education debt once he graduated and believed, like many others, that he had to pursue a subspecialty to make a decent salary; a career in primary care could not be lucrative.
Bias says that his family medicine preceptorship, a requirement of his medical school curriculum, was what made him realize he could pursue this career. His preceptor earned a generous salary his first year out of residency and had a well-run, business-savvy practice. Seeing this made it seem “easy,” Bias says. “It was the only reason I thought about family medicine.”
Now Bias looks forward to the day he has an established family medicine practice when he can volunteer to be a preceptor, passing on his positive experience for the next generation of physicians. “The preceptorship is not to teach you medicine; it’s to teach you about the real world of medicine, the business of medicine, the humanitarian side of medicine.”
Authorized through the Texas Education Code, the Texas Higher Education Coordinating Board oversees the three primary care preceptorship programs. THECB receives an appropriation from the state to cover administrative costs and student stipends—currently $1,000 for rural preceptorships and $750 for urban—and contracts with three organizations that operate the programs for each specialty: the University of Texas Health Science Center at Houston for family medicine, the Texas Chapter of the American College of Physicians for internal medicine, and the Texas Pediatric Society for pediatrics.
The Texas Statewide Family Medicine Preceptorship Program has been in operation for the longest of the three, having accepted its inaugural class in 1980. The General Internal Medicine Statewide Preceptorship Program and the General Pediatric Preceptorship Program were both created in 1995. All together, the programs have placed nearly 9,000 students in primary care preceptorships across the state.
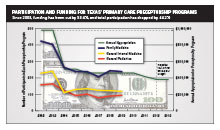
While impressive, funding depends on the will of the Texas Legislature, and budget reductions over the past decade have put a noticeable dent in student participation. The most damaging cut to the preceptorship programs came during the 79th Texas Legislature in 2003. This was the case for most state initiatives at the time, says Stacey Silverman, Ph.D., THECB senior director of academic research and grant programs. In her previous position at the coordinating board, Silverman oversaw the preceptorship programs, and she was on staff when funding was cut in half from $1.94 million in fiscal years 2002-2003 to $997,000 in 2004-2005.
This cut occurred as a result of the $10 billion state budget deficit lawmakers faced in 2003, caused mainly by the national economic recession and low sales tax revenue. “In the second year of the 2002-2003 biennium, we had to reduce funding,” Silverman says. “For fiscal years 2004-2005, the Legislature again faced a shortfall in funding and as a result, many if not all [state] programs received funding reductions.”
Staff from the coordinating board and the primary care preceptorship programs brainstormed ways to deal with the cut, responding with streamlined administrative tasks and reduced student stipends.
More importantly, the reduced funding meant the programs could only match a little more than half of the students previously enrolled, causing the number of students participating in the preceptorships to plummet from just over 800 in fiscal 2003 to roughly 500 in fiscal 2004. They received another 10 percent cut in 2006-2007 to $904,000 where funding has remained until the current biennium. With no new money available, student participation has remained flat for the most part, standing at 452 in fiscal 2009.
In the face of the current budget shortfall, state leaders asked all state agencies in January 2010 to propose a 5 percent overall reduction in their general revenue spending for the 2010-2011 biennium. While some THECB programs were cut completely, the statewide preceptorships withstood the baseline 5 percent reduction, which totaled just over $45,000 and will come out of the programs’ 2011 budgets. The effect on GIMSPP alone will mean the number of medical students able to be matched into an internal medicine preceptorship with funding will drop from 90 in 2010 to about 40 in 2011, according to staff.
Now state leaders are preparing for an even worse budget scenario for 2012-2013—a shortfall that experts predict could fall between $18 billion and $22 billion, or 10 to 12 percent of the state’s total $180 billion budget—and have asked agencies to make further reductions in their legislative appropriation requests, or LARs. As a result, THECB’s proposed 2012-2013 LAR trims a combined 10 percent from the preceptorships for the next biennium, which could cut 85 more spots from the program.
In total, if this cut goes through, funding for preceptorships will have decreased 60 percent in 10 years, not accounting for inflation, without any recovery of lost funds.
TAFP lobbyist Marshall Kenderdine stresses that the reason for the reductions is not lack of knowledge or support for the program. In the latest budget reduction, THECB ranked the preceptorships high on their priority list of programs to spare. “It’s not that any legislator is against funding preceptorship programs, it’s just that there are a number of programs competing for a limited number of state resources,” Kenderdine says.
Fortunately, says Gene Stokes, M.D., chair of the committee that oversees the GIMSPP, the programs have the data to prove their worth. Speaking specifically about GIMSPP, “It does increase the number of applicants to primary care programs, it does increase the number of primary care doctors trained who eventually stay in Texas, and it does have an influence on the number of doctors who enter rural and underserved areas.”
Each year, students and preceptors fill out an exit survey about their experience. According to these surveys, of the more than 1,400 medical students who completed a general internal medicine preceptorship between 1999 and 2006, 40.6 percent of them enrolled in an internal medicine residency program, 26.4 percent of them said they intended to practice primary care, and 82 percent of them intended to stay in Texas.
Pediatrics report similar findings: 37 percent of the almost 1,400 medical students who completed a pediatric preceptorship between 1999 and 2009 entered a pediatric residency and 62 percent stayed in Texas. For family medicine, of the 238 medical students who completed family medicine preceptorships in 2009, 93 percent said the experience made them more receptive to primary care as a career.
A study by UT Houston published in the Journal of Academic Medicine in 2004 took a critical look at the family medicine program between 1992 and 2000. The authors concluded that “the proportion of students choosing family practice residencies was significantly greater [among participants] than among nonparticipants.”
The authors tracked more than 10,000 students who graduated from eight Texas medical schools between 1992 and 2000, finding that 52 percent of them chose family medicine, general internal medicine, or pediatrics. Of the roughly 2,500 who participated in the preceptorship program, 27 percent chose family medicine residencies compared with 15.7 percent who chose family medicine without having participated in the preceptorship program.
In terms of increasing the primary care workforce, the authors found, “If the students who participated in the [TSFMPP] had selected family practice residency at the same rate as had those who did not participate, over 300 fewer students would have chosen family practice careers.” In essence, without the influence of the preceptorship program, the state shortage of primary care physicians would be even worse.
“These outcomes show that the only way to promote family medicine is to get into the medical schools and change the curriculum so the students have more exposure to family medicine, or to keep offering these programs where they get this really early exposure,” says Rachel Dorn, statewide coordinator for TSFMPP. “I’ve had several students who have told me their preceptorship completely changed their mind about family medicine, just having that experience they wouldn’t have otherwise had.”
Austin family physician Mark Hutchens, M.D., participates in the Texas Statewide Family Medicine Preceptorship Program.
Austin family physician Mark Hutchens, M.D., agrees, pointing out shortfalls in the nation’s medical school curriculum. “The nature of medical education in our country is that we’re more focused on specialty care and all of our training is done in care settings where they’re more focused on that,” he says. “I think most students don’t have an idea of what they want to do and they’re not exposed to primary care medicine as a whole until they finish their other specialty rotations.”
While these programs can’t solve the workforce crisis alone, they do have a significant role in correcting students’ false perceptions of primary care early in their medical careers, spurring interest in these specialties that they might not have considered previously. And these gains can be achieved with a relatively small investment by the state.
As Stokes points out, “This is incredible for $2-or-$3 million to have the kind of impact we can have on primary care in the state of Texas.” A specialist himself, he says he is “sold on the idea of primary care” and its ability to provide higher-quality, lower-cost care than can be provided by a group of specialists. “This is definitely the penny of medicine for the pound of cure. … [Legislators] have an opportunity to make an impact on the state of Texas and we can’t quite get them to hear this message.”
The Texas Primary Care Coalition, which includes TAFP, the Texas Chapter of the American College of Physicians, and the Texas Pediatric Society, asks the Texas Legislature to consider the future of the state’s primary care workforce and the economic benefit enjoyed by communities with access to high-quality primary care, and restore funding for the Texas Statewide Preceptorship Program to 2002-2003 levels. This would require investing $1 million per year, or $2 million per biennium. Kenderdine says, “It’s a small investment for a relatively large payoff, which also coincidentally helps to meet our workforce needs going forward.”
“In my opinion, I don’t think $2 million should be a ceiling,” Stokes says. “I think they ought to look at a $5 million investment. It’s such a small amount of the total [state] budget, but the impact can be absolutely incredible to our cause.”
While each of the three programs faces unique operation challenges to ensure an adequate volunteer corps of preceptors, student applicants, and staffing, they share a common worry: continued funding.
With further reductions, “we’d have to limit the number of preceptorships offered, limit travel money, and do less recruiting and promotion,” Dorn says. Reducing the amount of student stipends is not an option. “If we compromise the amount of stipends, we would have no student interest. Or we’d just have the students who are going to go into family medicine regardless. Our goal is to get the students who are on the fence and bring them in.”
Amy White, director of the pediatrics preceptorship, says decreased funding means the programs lose their edge. “The more students we get through the program, the more exposure students receive to the primary care field. The less money we have, the less opportunity we have to do so.”
“The physicians see it as the future of internal medicine and if this program gets cut, it would be devastating,” says Gena Girardeau, executive director of the Texas Chapter of the ACP. “A bigger concern is for the patients of Texas. If we don’t have enough internal medicine and primary care doctors, the general population won’t get the care they need or deserve.”
Download the Primary Care Coalition issue brief that supports continual funding of the Texas Statewide Preceptorship Program on the advocacy resources page of www.tafp.org.
Also, visit the webpages for each of the preceptorship programs: