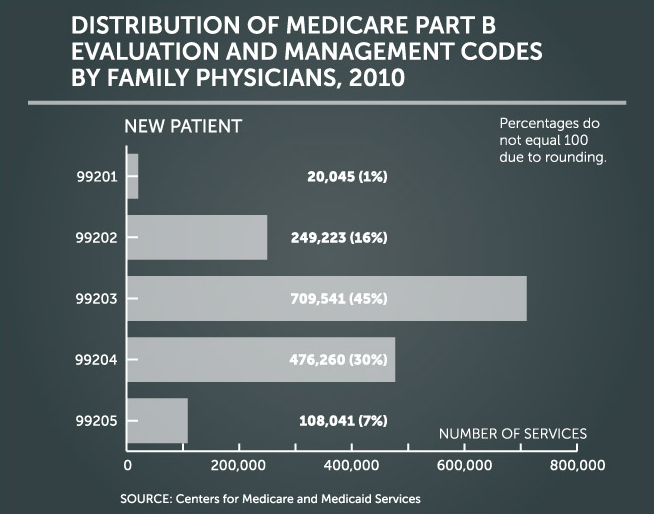
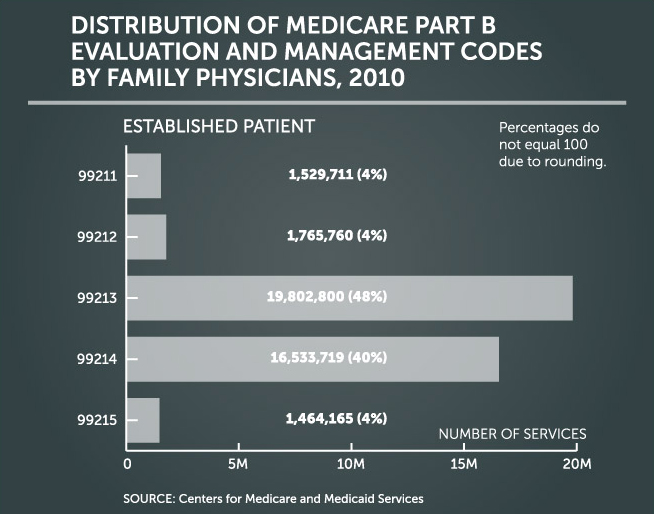
Recovery Audit Contractors: Distribution of E&M codes by FPs, 2010
Evaluation and management codes, the most common codes billed by family physicians, are more subjective than any others and therefore open to scrutiny. The graphs below display the sheer number of E/M codes billed to Medicare in 2010.
As Cindy Hughes, AAFP’s former coding and compliance specialist says, “an office visit for a middle-aged, obese female with multiple complaints and chronic conditions is scrutinized first on documentation of history, exam, and medical decision-making based on the payer’s interpretation of E/M coding guidelines; then someone other than the physician who was face-to-face with the patient may conclude that the documentation includes services that weren’t medically necessary for the complaints and conditions, and if any other services are provided at the time of the office visit, whether or not separate payment will be made for those.” That may be one reason why it may appear that physicians make more coding errors on E/M services than other codes.
AAFP sent a formal request to Medicare asking that the claims review for E/M codes not include the level of service reported due to the complexity of interpreting physician documentation to support the codes reported. CMS responded that the review of duplicate claims of E/M services was available during the demonstration and will continue to be available for review, but that the review of the level of the visit of some E/M services was not included in the RAC demonstration. CMS pledged to “work closely the physician community prior to any reviews being completed regarding the level of the visit” and to “provide notice to the physician community before the RACs are allowed to begin reviews of evaluation and management services and the level of the visit.”
Online resource
Go to the Compliance section of the AAFP Coding Resources page for a Code of Conduct and the OIG Compliance Plan for Small Practices